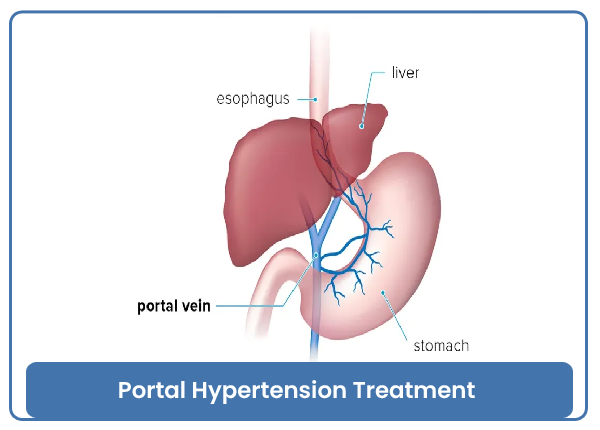
Portal Hypertension Treatment
Portal hypertension is a condition characterized by increased blood pressure within the portal vein, which carries blood from the digestive organs to the liver. This condition can lead to various complications, such as the development of varices (enlarged veins) in the esophagus and stomach, and it is often associated with liver cirrhosis. The goal of treating portal hypertension is to manage its underlying causes and prevent or manage complications.
Treatment Approaches for Portal Hypertension:
-
Treating Underlying Liver Disease:
- Alcohol Cessation: If alcohol-related liver disease is the cause, stopping alcohol consumption is crucial.
- Treatment of Hepatitis: Antiviral medications may be used to manage chronic viral hepatitis (e.g., hepatitis B or C).
- Managing Cirrhosis: For individuals with cirrhosis, addressing the underlying cause (e.g., viral hepatitis, nonalcoholic fatty liver disease) and providing supportive care is essential.
-
Medications:
- Beta-Blockers: Medications such as propranolol or nadolol may be prescribed to reduce portal vein pressure by decreasing the heart rate and blood flow to the liver.
- Vasoconstrictors: Octreotide or vasopressin analogs may be used to constrict blood vessels and reduce blood flow in the portal vein.
- Blood Pressure Medications: ACE inhibitors or angiotensin receptor blockers (ARBs) may be prescribed to manage portal hypertension-related complications.
-
Endoscopic Treatment:
- Variceal Band Ligation: Elastic bands are used to tie off varices, reducing the risk of bleeding.
- Sclerotherapy: Injection of a sclerosing agent into varices to cause them to shrink and scar.
-
Transjugular Intrahepatic Portosystemic Shunt (TIPS):
- A TIPS procedure involves the creation of a shunt (a small passage) within the liver to redirect blood flow and lower portal vein pressure. This is typically done using a catheter inserted through the jugular vein.
-
Surgical Shunt Placement:
- In some cases, surgical procedures may be performed to create a shunt that diverts blood flow away from the liver, reducing portal hypertension.
-
Liver Transplantation:
- For individuals with advanced liver disease, liver transplantation may be considered as a definitive treatment. This involves replacing the diseased liver with a healthy liver from a donor.
Complications of Portal Hypertension:
- Variceal Bleeding: Enlarged veins (varices) can rupture and cause life-threatening bleeding.
- Ascites: Accumulation of fluid in the abdominal cavity.
- Hepatic Encephalopathy: Cognitive impairment due to liver dysfunction.
- Spontaneous Bacterial Peritonitis (SBP): Infection in the ascitic fluid.
- Hepatorenal Syndrome (HRS): Kidney dysfunction in advanced liver disease.
The choice of treatment depends on the underlying cause of portal hypertension, the severity of liver disease, and the presence of complications. Management is often multidisciplinary, involving hepatologists, gastroenterologists, interventional radiologists, and transplant surgeons.
It is crucial for individuals with portal hypertension to receive regular medical monitoring and follow-up to manage their condition and prevent complications. Treatment plans are tailored to individual needs, and ongoing communication with healthcare providers is essential for optimal care.
Category : Portal Hypertension Treatment