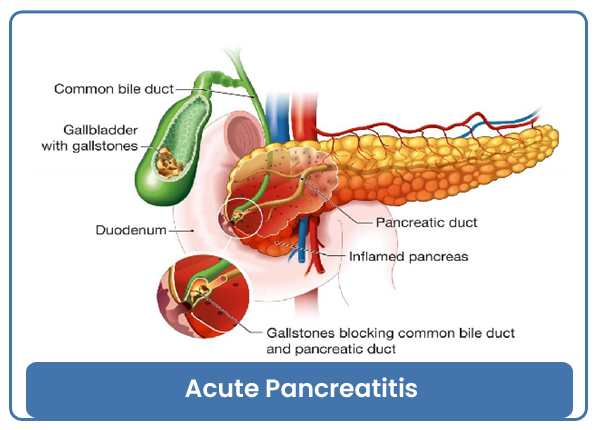
Acute Pancreatitis
Acute pancreatitis is a sudden inflammation of the pancreas, a gland located behind the stomach that plays a crucial role in digestion and blood sugar regulation. The inflammation occurs when digestive enzymes become activated while still in the pancreas, leading to damage to the pancreatic tissue. This condition can range from mild and self-limiting to severe, with potential complications.
Causes:
-
Gallstones: One of the most common causes, is gallstones can block the pancreatic duct, leading to inflammation.
-
Alcohol Consumption: Excessive alcohol intake is a significant risk factor for pancreatitis.
-
Trauma: Injury to the pancreas, such as from surgery or an accident, can trigger inflammation.
-
Infections: Viral or bacterial infections affecting the pancreas can cause pancreatitis.
-
High Triglyceride Levels: Elevated levels of blood fats (triglycerides) can contribute to pancreatitis.
-
Certain Medications: Some medications, especially certain types of antibiotics and immunosuppressants, may be associated with pancreatitis.
Symptoms:
-
Upper abdominal pain: The pain may be severe and radiate to the back.
-
Nausea and vomiting: Often accompanied by abdominal tenderness.
-
Fever and increased heart rate: Inflammation can lead to systemic symptoms.
-
Jaundice: In severe cases, there may be yellowing of the skin and eyes.
Diagnosis:
-
Blood tests: Elevated levels of pancreatic enzymes, such as amylase and lipase.
-
Imaging studies: CT scan or abdominal ultrasound to visualize the pancreas and detect inflammation.
-
Clinical history and physical examination: Including assessment of symptoms and potential risk factors.
Treatment:
-
Pain Management: Pain relief is a key component of treatment, often achieved with medications.
-
Fasting: Giving the pancreas a break from digestion by restricting food intake for a few days.
-
Fluid Replacement: Intravenous (IV) fluids to prevent dehydration.
-
Underlying Cause Treatment: Addressing the specific cause, such as gallstone removal or alcohol cessation.
-
Nutritional Support: Gradual reintroduction of food and dietary changes to support recovery.
In severe cases, hospitalization may be required, and complications such as infection, pancreatic necrosis, or organ failure may necessitate intensive care.
Acute pancreatitis can vary widely in severity. Mild cases may resolve with conservative management, while severe cases can be life-threatening and require prompt medical intervention. If you suspect pancreatitis or experience severe abdominal pain, it is crucial to seek medical attention for a proper diagnosis and appropriate treatment.
Category : Acute Pancreatitis